We left Kumasi at 4:30 in the morning, and slept soundly as our expert driver and navigator led us through thick fog and heavy traffic, around familiar potholes, and past Liberian refugee camps. Our rush back to Accra was temporarily interrupted by policemen who noticed the speeding bus, but we paid the ticket “on the spot” and were back on the road on time to meet the surgical team in the Reconstructive Plastic Surgery and Burns Centre at Korle Bu Hospital.
The surgical team was gracious enough to wait for our arrival to begin surgery for several cleft lip and palate patients. Our group divided into three teams based on academic and clinical experience with cleft palate, and took turns observing Dr. Paintsil, Dr. Laing, and Dr. Ampomah repairing cleft palates for an infant and then a six-year-old.
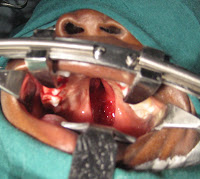
As the first group observed Dr. Paintsil, he told them the patient’s background, and explained each step of the surgery. This group observed the repair of the infant’s cleft palate, who had previously had his lip repaired. Dr. Paintsil told the students that the child seemed to have typical cognitive development, and that since the repair was being done so early, he would most likely speak almost typically after he healed. Dr. Paintsil also introduced the students to the other professionals in the room, including the scrub nurse, Comfort, the orthodontic surgeon, and several medical students. The students in our group were impressed and inspired by Dr. Paintsil’s thorough knowledge of his craft. He was very savvy about speech production, and pointed out all relevant anatomical structures to the students, including several muscles, the lateral pharyngeal walls, and the tonsils. He explained that since the oral muscles are so important for feeding and speech, he uses non-absorbable stitches when repairing the muscles to ensure that the closure will hold.
The teams from our group that were not observing surgery were upstairs providing speech, language, and feeding therapy to the cleft lip and palate patients and their families. The students saw several children of varying ages, and one adult. When evaluating the children, the students would often first ask the parent to open their mouth, and would look at it with a flashlight. After seeing their parents cooperate with the student-clinicians, the children were more comfortable and willing to show us their clefts or repairs. Many of the youngest children had already had a lip repair but were waiting for their cleft palate repair, and sessions with these children mostly consisted of feeding therapy and recommendations to encourage production of sounds that can be produced correctly even with a cleft, such as nasal sounds and vowels.
Many of the older children had already had complete repairs, and were given articulation evaluations and recommendations. One child, age six, was a student-clinician’s dream come true. She had had a cleft of the anterior part of the secondary palate repaired two months earlier, and was otherwise very healthy. Her cleft had been discovered because her speech “didn’t sound right” to her parents or teacher. She was very intelligent, as was her father, who had been listening carefully and noticed her difficulty producing /s/ and /t/ sounds. The student-clinicians also asked her to count and say the ABC’s, and discovered that she had difficulty producing “ch,” “sh,” and /f/ sounds. She watched the student-clinicians very carefully as they showed and explained to her correct tongue placement and airflow techniques, and was able to imitate every sound correctly after only a few tries. Her father had also been watching closely, and practiced cueing her correct sound productions using the student-clinicians’ techniques. The students gave the family lists of facilitative sound sequences and words to use alone and then in sentences, so she could practice her speech at home. The shy child smiled several times as the session concluded, and her father beamed back proudly.
 |
| Dr. Albert Paintsil |
 |
| Dr. Laing |
It was a long day, and our dinner that night was the first meal we ate. But thanks to our ever-expanding knowledge base and cultural awareness, most of us already felt fulfilled.
-Charity Delsie
-Charity Delsie




Thanks for your work and help bringing cleft palate surgery to the children that need it. The conference sounds like it was a great place to share ideas on cleft lips and palates.
ReplyDelete